The number of cases of "superbugs," as researchers call them, has been grown steadily in recent years. When antibiotics are used for non-bacterial illnesses, or when prescriptions are not taken for the full cycle, the bugs that endure pass on their drug-resistant traits to subsequent generations. New research from Cambridge should help hospitals control the spread of superbugs. It has been shown for the first time how transmission of the bacterial infection can be tracked between people in different continents and from patient to patient in a single hospital by using DNA sequencing technologies.single hospital by using DNA sequencing technologies.
The number of cases of "superbugs," as researchers call them, has been grown steadily in recent years. When antibiotics are used for non-bacterial illnesses, or when prescriptions are not taken for the full cycle, the bugs that endure pass on their drug-resistant traits to subsequent generations. New research from Cambridge should help hospitals control the spread of superbugs. It has been shown for the first time how transmission of the bacterial infection can be tracked between people in different continents and from patient to patient in a single hospital by using DNA sequencing technologies.
!ADVERTISEMENT!One of the most vexing superbugs is methicillin-resistant Staphylococcus aureus, or MRSA. This bacteria used to be acquired mostly in hospitals, but now more people are getting it elsewhere. It can cause skin infections, severe bloodstream infections and even death.
If regular drug resistant bacteria weren't bad enough, some bacteria have become multidrug resistant (MDR).
What is not controlled or killed by an antibiotic can cause harm and even death.
Researchers at the Beth Israel Deaconess Medical Center and Harvard Medical School studied the prevalence of bacteria resistant to three or more drugs over a six-year period. From 1998 to 2003, there was a significant increase in the incidence of patients carrying multidrug resistant (MDR) bacteria when they were admitted.
What causes this?
Antibiotics shut down unruly bacteria directly, police them until the immune system can rid of them or both. Each new antibiotic on the market works well at least for a few years. Those bacteria that survive antibiotic treatment will reproduce and their descendants are more likely to resist the antibiotic.
Knowing how the MRSA is transmitted can lead to suitable precautions to stop other people from becoming infected. In the past many populations were isolated reducing the spread of new pathogen. Nowadays disease can spread rapidly from almost any corner of the world.
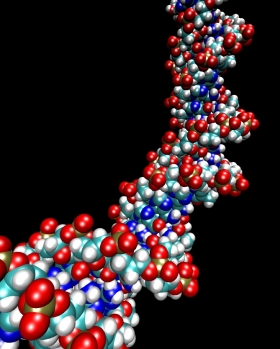
The Cambridge study used new DNA sequencing technologies on samples taken from people with MRSA across the world.
One of the authors on the study, Dr Sharon Peacock, professor of clinical microbiology, said: "Until now it has not been possible to examine transmission of MRSA between countries and within and between health care institutions.
"The fine scale discrimination that is now possible between two or more highly related MRSA strains means that it becomes possible to identify where strains have spread and implement control measures to prevent this from happening."
The sequencing and data analysis were performed at the Wellcome Trust Sanger Institute and Dr Peacock was involved in clinical interpretation of the data, as well as considering the future application of the technology.
She added: "Our research should inform global surveillance strategies to track the spread of MRSA."
"The implications for public health are clear. This technology represents the potential to trace transmission pathways of MRSA more definitively so that interventions or treatments can be targeted with precision and according to need."
Two very different sets of samples were used. The first contained 42 samples from people throughout the globe who became infected with MRSA between 1982 and 2003.
The second set was from a single hospital in north-east Thailand and comprised 20 samples from patients who developed the infection within seven months of each other and which were possibly transmitted from person to person.
Dr Simon Harris, from the Wellcome Trust Sanger Institute, the co-lead author on the study, said: "We wanted to test whether our method could successfully zoom in and out to allow us to track infection on a global scale, from continent to continent, and also on the smallest scale, from person to person."
The team also developed an evolutionary tree of MRSA by looking at samples from hospitals in North and South America, Europe, Australia and Asia over more than 20 years. The research suggests that the infection emerged in the 1960s in Europe.
For further information please see: http://www.admin.cam.ac.uk/news/dp/2010012201 or http://en.wikipedia.org/wiki/Antibiotic_resistance