The body mass index (BMI) is a heuristic proxy for human body fat based on an individual's weight and height. BMI does not actually measure the percentage of body fat. It was devised between 1830 and 1850 by the Belgian polymath Adolphe Quetelet during the course of developing "social physics". Body mass index is defined as the individual's body mass divided by the square of his or her height In addition to the many risk factors associated with poor health, reducing body mass index (BMI) will have a considerable and independent impact if you want to reduce the risk of developing ischemic heart disease (IHD). This is the key finding from new research, published in PLoS Medicine, which evaluated the causal relationship between BMI and heart disease in 76,000 individuals.
The body mass index (BMI) is a heuristic proxy for human body fat based on an individual's weight and height. BMI does not actually measure the percentage of body fat. It was devised between 1830 and 1850 by the Belgian polymath Adolphe Quetelet during the course of developing "social physics". Body mass index is defined as the individual's body mass divided by the square of his or her height In addition to the many risk factors associated with poor health, reducing body mass index (BMI) will have a considerable and independent impact if you want to reduce the risk of developing ischemic heart disease (IHD). This is the key finding from new research, published in PLoS Medicine, which evaluated the causal relationship between BMI and heart disease in 76,000 individuals.
!ADVERTISEMENT!
BMI, alongside age, smoking, diabetes, high blood pressure, high blood cholesterol levels, and individuals who have family history of the disease, has been long recognized as a risk factor for heart disease. Despite this, the actual causal contribution of BMI to disease risk has been difficult to quantify.
New findings from a collaborative effort between the Medical Research Council (MRC) Center for Causal Analyses in Translational Epidemiology (CAiTE) at the University of Bristol and colleagues from Copenhagen University Hospital, have revealed that an elevation in BMI of around 4kg/m2 across the life-course will increase the risk of developing the disease by 50 per cent on average.
Using genetic data from three large Danish studies — the Copenhagen General Population Study, the Copenhagen City Heart Study and the Copenhagen Ischemic Heart Disease Study — the researchers were able to use genetic variation known to be related to BMI to measure the true causal effect between this and IHD.
In observational estimates, the researchers found that for every 4 kg increase in BMI a 26 per cent increase in odds for developing IHD, while causal analysis identified a 52 per cent increase.
Dr Timpson, Lecturer in Genetic Epidemiology from the University’s School of Social and Community Medicine, said: "In light of rising obesity levels, these findings are fundamental to improving public health. Our research shows that shifting to a lifestyle that promotes a lower BMI (even if it does nothing else) will reduce the odds of developing the disease."
Professor Børge Nordestgaard, lead author of the study from the University of Copenhagen, added: "These findings are of key importance, as obesity linked to diabetes is the only major cardiovascular risk factor on the rise in North America and Europe, while smoking, cholesterol levels and hypertension have been decreasing."
The U.S. National Health and Nutrition Examination Survey of 1994 indicated that 59% of American men and 49% of women had BMIs over 25 (described as overweight).
Morbid obesity—a BMI of 40 or more—was found in 2% of the men and 4% of the women. The newest survey in 2007 indicates a continuation of the increase in BMI: 63% of Americans are overweight or obese, with 26% now in the obese category (a BMI of 30 or more).
There are differing opinions on the threshold for being underweight in females; doctors quote anything from 18.5 to 20 as being the lowest weight, the most frequently stated being 19. A BMI nearing 15 is usually used as an indicator for starvation and the health risks involved, with a BMI <17.5 being an informal criterion for the diagnosis of anorexia nervosa.
For further information see Article or Bristol BMI
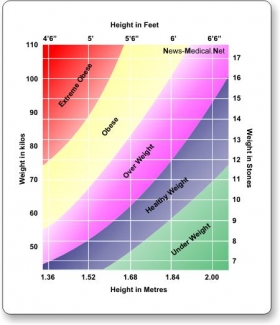
Chart image via Kansas State University